 In November 2017, a routine screening colonoscopy revealed
colon cancer—an unhappy surprise in anybody's book—and
I had my sigmoid colon removed in December of the same year
by a very talented colorectal surgeon. Thanks, Dr. Rad!
In November 2017, a routine screening colonoscopy revealed
colon cancer—an unhappy surprise in anybody's book—and
I had my sigmoid colon removed in December of the same year
by a very talented colorectal surgeon. Thanks, Dr. Rad!
Pathology showed that the cancer had spread into a few of the
local lymph nodes: I had stage 3a colon cancer, and chemotherapy was
indicated for me in early January. Happy New Year!
This is the story of my journey from a patient's point of view
with things I wish I'd have known at the time. At all times I had
good medical care, but there were all kinds of things that
would have improved my day-to-day life; I'm hoping to share this
with you.
I cannot emphasize enough: this is not medical advice.
I am not qualified to do anything other than tell my own story,
and at Every. Single. Point. you must defer to the judgment
of your medical team. My advice is typically practical, not clinical.
This is also based on my own personal circumstances, which may not
match yours; I'm a 55 year old male, in good health, with no prior
family history of colon cancer, and receiving
the FOLFOX6 chemotherapy regime.
If your regime is different, your
health is different, your oncologist is different, your infusion center
is different, or if you are not me: your mileage may vary, though some parts may still apply.
In addition, each infusion center (and oncologist) has their own
protocols and procedures, so even if you're on the same drug
regimen as me, it might not play out the same way.
What I also have going for me was an exceptionally positive
attitude, superb insurance, a very deep bench of friends, and
of course a wonderfully supportive wife. I'm self employed, which
gave me great flexibility with errands and naps.
As I write this, I'm on chemo Round 11 (of 12), and I'm not sure I could be any more lucky.
Update: July 2018; I'm now through all my 12 rounds of chemo. Whew!
Update: Sept 2019: Chemo long over, multiple blood tests and CAT scans show all is well. Yay!
Update: Jan 2020: All is still well, and I'm now making updates at the bottom chronologically
rather than update this in place. If you've visited this page before, skip to the bottom.
Disclaimer: Throughout this note I'll provide links to many references
to Wikipedia, and in some cases
to specific recommended products at Amazon.com or other vendors, but I'm not
selling anything and don't get referral/commission from anybody.
Preparing for your journey
Everybody has their own habits and coping mechanisms, and in my
case, as a voracious consumer of science, I empowered myself by
diving deep into the medicine and chemistry of cancer, pretty much
geeking out on details.
Though many of the details really did help me understand what's
going on in my body, making sense of a side effect, many of the
technical details were little more than bar trivia tricks, as
there's nothing you can usefully do knowing that
(say) 5-Flourouracil is a
thymidylate synthase inhibitor.
But even those who don't have the interest that way
can still help themselves: the internet is
a wonderful resource for those going through this, and Google
will be your friend.
Cancer support websites abound, where you can find out that
others are going through the same thing as you: this goes a long
way to not feeling alone.
However your personal inclinations, I can offer a few pieces
of general advice.
- Journal / Keep good notes
- I keep a file on my computer, and I make notes virtually
every day, and this has been incredibly useful.
- Initially I made notes of every phone call I made to
a doctor or insurance carrier while setting up my surgery
and planning for the oncologist: This is really helpful
in case a provider is dropping the ball.
-
That kind of phone-call detail may not come up so much once
you settle into a groove with chemo, but it's then that you
need very good notes on how you're feeling, what you took,
how side effects are going, and all that.
-
If you're going through 12 rounds, you really want to identify
patterns, especially the cumulative side effects. Being able to
tell your doctor that the yuck started to wear off on Day 5 but
the neuropathy hung on until the middle of the "off" week means
they will give you better care.
-
Going to your doctor with a good record of your symptoms is important.
- Bring somebody with you to the first oncologist appointment
- There's so much information to learn, you simply cannot keep
it all in your head even if you take good notes and the doctor explains
well and gives handouts. It's just too much.
- Having a spouse or a friend means they will remember things you
don't, and will ask questions you didn't think about. This is so,
so useful.
- Educate yourself from reliable sources
- The internet is a mixed bag of information: some great
resources, and some not so great, and it can take some digging
to sort it out.
- Personally, I have a strong (but informal) background in
science and have a very good BS detector, so I'm able to easily
separate the good data from the nonsense.
-
And there's a lot of nonsense from all kinds of crackpots,
including those proposing that amazing watermelon cure from
Mexico where you can "detoxify" your way to being cancer free.
-
One I'll call out by name to avoid is Food Babe:
she has a great talent for hyping an entirely science-free position into bad
advice. My blog post
on one of her screeds shows how to think critically, and hopefully
will fine-tune your own BS detectors.
-
Dr. Oz is also to be avoided for any kind of medical advice unless
you're looking for snake oil.
-
You'll also receive well-meaning advice from friends that
it's all a conspiracy by Big Pharma and you should never let
them put that poison in you, instead opting for holistic remedies.
This opinion is often delivered passionately and entirely in good faith.
-
 You should of course consider all legitimate treatment
courses, but I'm firmly in the camp of science and modern
medicine, so I thank the giver of this advice for caring about
me so much, and letting them know that I am very comfortable
with my decision given that I really do understand this stuff.
You should of course consider all legitimate treatment
courses, but I'm firmly in the camp of science and modern
medicine, so I thank the giver of this advice for caring about
me so much, and letting them know that I am very comfortable
with my decision given that I really do understand this stuff.
-
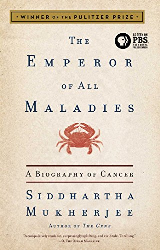
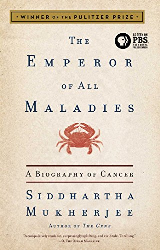
Super reliable source:
I'd be remiss if I did not recommend an outstanding book:
The Emperor of All Maladies: A Biography of Cancer.
This is not a self-help book, not how to avoid cancer by eating right, or anything like that. This is a deep background on cancer, and it's
absolutely fascinating. The author is an oncologist and a damn fine writer: he won the Pulitzer Prize for this book.
-
It's really for the general public, not just cancer patients; I had read it 5 years ago, then re-read it when this
all hit the fan for me, and understanding how cancer works (and how cancer medicine works) can go a long way to
removing a bit of the mystery of this disease. Mysteries are scary: this book helps. Your close circle should all
read this book.
-
And as I write this, I discovered that Ken Burns has created a documentary based on this book: this I gotta see!
- Accept help from friends
- To the extent that you really can use some assistance:
a ride to a medical appointment, somebody to cook for you or make a run to
the grocery store, to sit with you in chemo for company.
Accept their help.
- People commonly wish not to be a burden,
but this is not the time for that. You're dealing with
cancer, you have people who want to help you, and it's a gift
to them to accept their help.
-
Really, it's ok for this to be all about you for a while. Own it!
- Consider making yours a public journey
- Everybody gets to decide if or how to share a private medical
condition, but for me, it was helpful to share this with my wide
circle of friends on Facebook.
-
Unless this is truly a confidential concern shared only with very
close family, your friends are going to wonder how you're doing,
and regular posts make it really easy to
keep them all in the loop. You'll still get asked about it, but
it saves a huge amount of time trying to remember what
you told to whom.
-
This is extra helpful if you actually could use assistance: you
can post your request for help, and you'll likely receive numerous
offers.
-
So many friends have told me how much they enjoy following
my progress, reading the geeky stuff, and how much they want
me to keep posting it.
-
In addition, colon cancer is highly preventable, and we can use our
experience to encourage others to get their colonoscopy. I've had
many friends report they finally got off their (ahem) butt
and got it done. Maybe we can save a life?
-
But this is a very, very personal decision, and the only one to
whom you owe complete details is your doctor (though a spouse
is a close second).
- Expect to feel overwhelmed sometimes
- Most people in this position had it drop upon their heads
suddenly and unexpectedly, and it's an enormous amount
of stuff to just absorb. The combination of the unfamiliar
medical information, the unpleasantness of the regimen, and the
wonder what your future holds—all of this is normal.
- Added to that are those with a limited local support system
or with unusually bad reactions to treatment (or with grim
prognoses), it's easy to see how this could give anybody
pause.
- Share your journey with trusted friends, ask lots of
questions of your doctor and nurses, and do what you can to
clear up mysteries: these all take a weight off. And a good
cry now and then doesn't hurt either.
-
Almost everything about this Tech Tip is here to help make it
an easier journey for you; feedback is welcome.
The FOLFOX6 Chemotherapy Regimen
Variants of the FOLFOX
regime is pretty much the standard of care
for colon cancer at most stages, and because my surgeon believes
he got all the tumor, my chemotherapy is
adjuvant therapy,
which is just insurance in case bits are brewing elsewhere too small to be detected.
The FOLFOX protocol is 12 rounds of two weeks each,
where you'll visit an infusion center on Day 1, spend a few
hours getting some of the drugs, then go home with a pump
attached to your port, then return on Day 3 to be disconnected.
The rest of the time you recover. Rinse and repeat.
The three main meds of this regimen are:
- FOLinic acid
(aka Leucovorin); it potentiates the flourouracil but is not a chemotherapy agent itself.
- Flourouracil,
aka the well-named 5-FU (say it aloud!)
it's a chemotherapy agent that gums up DNA replication.
- OXaliplatin;
another chemo agent that gums
up DNA, but this has the side effects you worry a lot about.
Much more on this later.
I saw my oncologist once a week for the first couple of rounds,
but he made it every other round once I settled into a good rhythm.
My doctor also put in an order for standing blood tests
which I had to handle on my own with a local lab. These are
in addition to the infusion-day blood tests they run automatically.
Variations abound: I am on FOLFOX6, but there's also FOLFOX4 and FOLFIRI,
and there will surely be others available. The ones I named are all on a similar two-week cycle, but I'm only really speaking of
FOLFOX6 in this tip.
Your Port
Because FOLFOX therapy requires you to take home a pump for a couple of days,
there's no way it could ever work with an IV line in the crook of your arm
or in your wrist. It would be a mess.
So I believe the standard of care is to have a General Surgeon implant
a "Smart Port" (aka Port-A-Cath, a few other names too) under your skin
in your upper chest, which provides easy access to the bloodstream.
Mine took 10 minutes to implant under local anesthesia, it's common
for patients to drive themselves to and from the procedure: easy business.
You can't really see the port itself in this picture, I've marked the location
with a red circle, and the two incisions were used by the surgeon
to make it so:
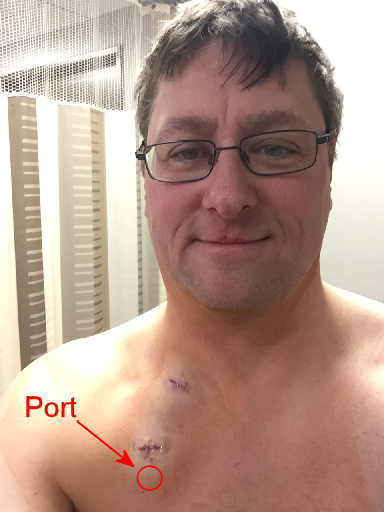
The flouroscope shows it inside:
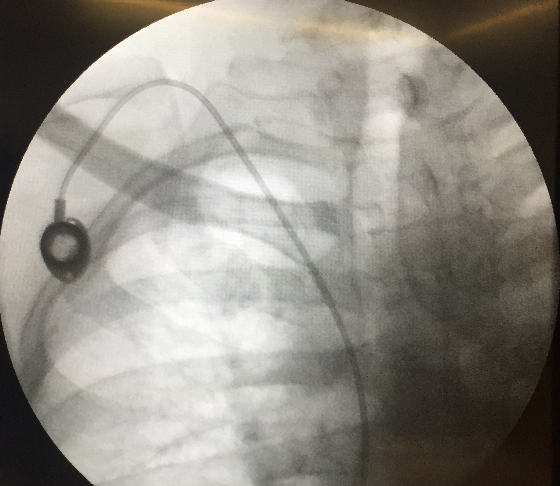
I really like my port; no getting poked in the arm every time.
For the first coupla days after implantation I had to cover it
while showering, but it was easy to manage.
I call mine "My USB port", and note that it's titanium for enhanced performance :-)
There are two action items I'd like to recommend regarding
infusion day with your port:
- Easy access for the nurses
-
The nurses have to get access to the port a few times, and
it really helps if you have a shirt that can unbutton all the way.
They can work around a t-shirt, but it's more awkward for them (and you).
-
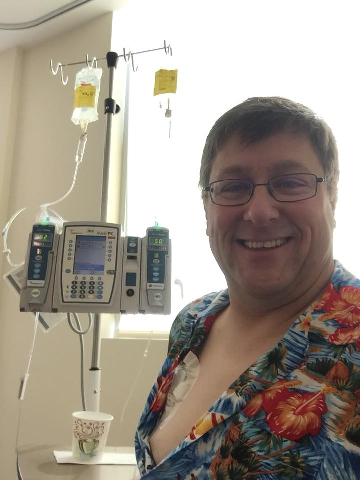
I've made it a point of wearing a Hawaiian shirt every time
just to liven up the place: the nurses (and patients) seem to enjoy it,
and it's all part of a positive attitude.
-
Here we see the infusion pump (not the take-home one!) hooked up to
my port, along with my festive attire:
-
- Numbing your port
-
The port is just under the skin, and it's pierced with a special
non-coring needle, and this is more or less like most other IV
access pokes.
-
Ask your oncologist if
EMLA cream
is right for you: this is a lidocaine type numbing cream you put on the skin
over your port around an hour before your
infusion to numb the area. It's super cheap and totally safe and many oncology
practices prescribe this automatically.
-
Mine didn't, and I was thankful a nurse friend suggested it.
-
You should cover the cream to keep it off your clothes, but
a regular Band Aid has a cloth-type patch that will soak it up
instead of going into your skin, so I use the same bandages that hospitals use:
-
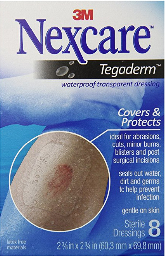
-
Tegaderm bandages;
about $6 for a set of 8 (get 2 boxes to cover 12 rounds).
-
You'll just put a small dab of the cream in the middle of the
clear sticky area and put it on your port. The nurses see
this all the time.
-
Update: I understand that some infusion centers
use a numbing spray on the port prior to puncture, which
achieves the same thing.
Update: One patient who had his port installed the same
place as mine has reported pain/discomfort when turning his head,
apparently because it's tugging on the tube under the skin. You
can't really see the tube under my skin, but you can under his.
I don't know if there are different techniques used by different
surgeons, if his was done poorly, or if I just got lucky.
Update Oct 2018: My port was on the right side so didn't interfere with
the seatbelt for driving—yes, I drove while connected to the pump—but
a helpful reader who had hers on the left side found that a kind of padding
around the seat belt helped.
Yes, of course there is such a thing: Chest Buddy Seatbelt Cushion (link to Amazon)
The Infusion Cycle
I have experience with two infusion centers in Orange County, California,
but there are likely many variations; you'll get the lay of
the land with yours at your first visit.
- Day 1 - infusion
-
I show up at 8AM at the local infusion center,
and on this day you're pretty much dealing with nursing
staff, not doctors. These are specially-trained oncology
nurses, plus there are often nursing assistants and possibly
even volunteers.
-
You'll step on a scale as you enter because the chemo meds
are based on height and weight, then off to a comfy chair
where routine vital signs are taken.
-
A nurse will access your port with a special needle, and they do this
one time only during your visit.
It hurts just for a second, it's no big deal (especially if you have
used the EMLA cream). The port is great.
-
The nurse will draw blood samples for testing to make sure you're healthy enough
for chemo: if your bloodwork is out of whack, they'll call
the doctor to see what they want, and in some cases they
may defer your infusion entirely until things normalize. I was deferred
twice for low plateletes, and others have been deferred from low white cell counts.
-
Then come the meds:
-
- IV Saline for hydration while waiting for the labs
and the pharmacy.
- If labs are good, pre-meds start: Zofran
(ondansetron) for nausea, plus a steroid to help the Zofran. This is maybe 20 minutes.
-
Then 2-hour infusion of Oxaliplatin and Leucovorin.
-
Flush the line with regular saline to make sure all the "good stuff" makes it inside.
These meds are crazy expensive and they're not going to leave any in the tubing.
-
They hook me up to the take-home pump with Flourouracil,
put it in a fanny pack, make an appointment for disconnection on Day 3,
then I hit the road.
-
The whole time I'm sitting in a comfy chair with my laptop,
I don't feel anything from the meds, they bring me water and
snacks and check on me: it's really quite pleasant.
-
My typical infusion Day 1 is around 4.5 hours, but it was
higher before we all got into a rhythm.
Allowing for 6 or 7 hours for your first time might not be
a bad idea: there's lots of 'splaining going on.
-
Some patients have visitors to keep company, I didn't need
that or really even want that: it's nice quiet time for me to
get some work done.
-
Note that not all patients are in there for the same thing, not
even all of them are chemotherapy patients. But you'll start to
recognize a few of the patients over time, and of course you'll
get to know the nurses really well.
- Home days 1/2/3
-
I'm toting a pump around for 46 hours, and because I work at home
it really does simplify my life. It's no problem to go out,
I just have a tube running from the fanny pack to my shirt,
and nobody's ever asked me what it is.
-
I did put orange racing stripes on mine to make it go faster :-)
and it a bit more festive, and I've never been self-conscious
about it while I was out and about.
-
Showering is inconvenient but doable: more on that later.
-
Sleeping wasn't any problem for me mechanically, in part
because I also wear a CPAP mask for apnea, so this didn't make
it any worse at all.
-
But because the steroid causes insomnia, I always take
a sleep aid on days 1 and 2, at least.
- Day 3 - Disconnect (aka Disco Day!)
-
I return to the infusion center 46 hours after my pump started,
and it's a brief visit: the nurse flushes the line, disconnects
the port and covers it with a bandage.
-
Here is where there can be variation: in my case, I get a shot
of Neulasta,
a "colony stimulating factor" that boosts white-cell production in the
blood to make up for the collateral damage from the chemo.
-
Neulasta is an amazing molecule, but it's crazy expensive, something like
$5000 per shot with insurance negotiated rates (maybe even more than $15000 "retail" cost), and not all insurance covers it. There are other therapies
and some patients just choose to skip it in any case without consequence.
-
I have skipped Neulasta once as an experiment, and at the start
of the next round found that blood work was a little low
but still ok for infusion. Always follow your doctor's
guidance on this.
-
Then it's time to go home after making the next infusion appointment,
a free man without pump in tow.
-
I had a personal reward ritual driving home from disco day to stop at
Arby's and get myself a huge roast beef sandwich. I almost never have fast
food, but with all the crap going on, this was a special treat.
Now the active part of the cycle is over, so it's biding your time
until the next round. Everybody responds differently, but for me
I found the neuropathy symptoms starting on the first day, with nausea
and yuck kicking in late day 3 and all day 4.
Once the "off" week arrives, there's essentially no more yuck for me
and only very minor neuropathy side effects, but I still write this
all down every day.
Let's drill down to some side effects.
Side Effects
I believe that everybody has some side effects, there's
just no escaping it, but there's a very wide variation in body
response and seriousness of side effects.
My understanding of chemotherapy is that FOLFOX is not nearly as
unpleasant as other kinds of chemo (breast cancer, for instance, is
a much worse experience than this), so in some respect we have it
easier than many others.
My doctor has told me, and I have confirmed elsewhere, that
severity of side effects does not correlate
with effectiveness of chemo. I always took this to be a relief
that you did not somehow have to hope for a bad time in
order for the chemo to be effective.
- Hair loss
- It is uncommon to lose your hair under FOLFOX; good news!
There may be some thinning, but I still have a full head of hair after
9 rounds. Edit: still full hair 18 months post-chemo.
-
I couldn't care less about my own hair loss, but understand this is
a very emotional issue for many, and we can be thankful we are
generally spared this.
-
In regimens for other kinds of cancer, hair loss can start on round one.
- Nausea and Yuck
-
Everybody expects nausea during chemotherapy (and radiation if your
regime includes it; mine doesn't), but this doesn't go far enough to
describe it.
-
The Yuck is an overall feeling of malaise, a crappy lousy feeling
that makes you feel bad all over even without the nausea, and for me
it starts mildly on Day 1.
-
I've been at a loss to describe it, and the closest I can come is that it's a bunch of
prodromal symptoms that
never materialize: you feel a headache coming on but don't get the
headache, you feel the flu coming on but don't get the flu.
-
It's just a big bundle of yuck that you really, really want to go away. A lot.
- Peripheral Neuropathy / Cold Sensitivity
-
This is the one to pay attention to: it's a tingling or pain in your hands
and feet, often provoked by cold, so if you reach into the fridge to grab
a can of soda, you'll feel a nasty zing of pain in your fingers.
-
Caused by the oxaliplatin, the cold sensitivity shows itself while
drinking a cold drink: it feels like liquid cactus in the back
of the throat and is very unpleasant. I've switched to drinking
room-temp water, and even that sets it off sometimes.
-
IMPORTANT: though nausea and yuck goes away completely after
chemotherapy is over, the peripheral neuropathy is cumulative and is likely to persist
after therapy ends, possibly fading away over months. And for some,
the symptoms become permanent. Yikes!
-
This is why it's so important to keep really good notes of how you feel
in every round and report it to your doctor so they can modulate
the dose down, especially if the symptoms continue into the "off" week.
-
The doctors typically speak of "activities of daily life", such as
buttoning a shirt, but for me, the peripheral neuropathy mainly
impacts my typing on a keyboard; that's my whole life (as
I type this now, my hands are cold and tingly, and it definitely slows me down).
-
In my case, these symptoms were troublesome enough that my doctor reduced
the oxaliplatin to 75% by the fifth round, and to 50% ih the tenth round, and it helped a lot.
We're basically playing "chicken" with oxaliplatin by planning for how it will be
six months after chemo.
-
Update for round #10: Up to this point, all the neuropathy symptoms
were acute, in the sense that they emerged right after infusion, and then faded
as the round progrssed. But my Round #10, the chronic neuropathy symptoms
started to come into play: these are milder but hang around longer and are not
so related to cold. It's hard to describe, but it just feels like this is
the kind of thing that will hang around longer.
-
These symptoms are not troublesome for me at all, but their emergence lags
the treatment, and we expect them to continue growing even after chemo stops, after
which the curve tips over the top and heads back down. The big question is how far
down will it go. We'll find out.
-
The good side, though, is that cold sensitivity to liquids completely went away,
so I was able to drink ice water at any time, and I suspect that better hydration
may have helped make round #11 easier for me.
-
Update for Round 12: the neuropathy has increased markedly, and it's for sure
not related to cold sensitivity. It's become painful and unpleasant, though not enough
to keep me from my work. I do expect it to continue to ramp up after the yuck is over,
but we have no way of knowing how it will progress.
-
The main impact has been trying to sleep: toes are very sensitive to even the light
touch of sheets, and it's not easy to get comfortable.
- "First bite syndrome"
-
Related to the peripheral neuropathy above, but a separate item because I added this
in Nov 2020 when I learned about it from two different people on the same day.
-
First Bite Syndrome is pain/spasms in the jaw muscles when taking the first bite
of food during a meal, with the sensation decreasing through the meal but coming back
after a break.
-
It might be on both sides or just one side, but it's related to muscle movement
part of eating and not the tasting part. It's said to be uncomfortable, and though
I'd not heard of it before, looking back I might have had a mild case of it but
it apparently wasn't prominent enough for me to investigate.
-
I'm pretty confident this is due to the always-helpful oxaliplatin, showing up
just after infusion, and fading away over the course of the cycle. I don't think
it's one of the permanent neuropathy side effects, but of course you should
always take good notes on when the symptoms start, how serious they are, and when
they start to face away: this is very important that you record this for your doctor.
- Mouth sores
- This didn't happen to me, but it's common enough that the nurses ask me
every time. They will recommend some kind of saline rinse to have ready in case
the problem arises, but I've not been there myself.
- Weight gain, but not really
-
The steroid they gave me during Day 1 infusion caused water retention,
so I would typically gain 5 or 6 pounds over 2 days (!!), but it always goes
away right after. It's alarming but not something to be concerned about
(but still report it to your doctor).
- Day 1 Insomnia
-
Our friend the steroid will also keep you crazy wide awake on day 1,
it's just one of the side effects, and many can make use of a sleep aid.
In any case, talk to your doctor in advance so you're ready on
the evening of Day 1; some sleep aids are more appropriate than others.
- Constipation / Diarrhea
- Your colon has been through a lot during surgery, so you've probably
already gotten a fair handle on your own digestive system, but the chemo
will definitely stir it up with one symptom or the other.
-
Patients who get diarrhea have to pay special attention to remaining
hydrated, but it never happened to me. I had the "slow" version of
symptoms and constipation was an ongoing struggle for quite a few
rounds.
-
It's hard to describe just how big a quality of life issue severe
constipation can be: chemo hasn't made me throw up due to direct
nausea, but constipation has. It can get really bad, especially
with the speed-up/slow-down that comes with use of the very effective
Milk of Magnesia.
-
Fortunately, my family doctor put me on a regimen that worked super
well for me, so I've been a "regular guy" for weeks now, and it's just
so nice to have this be a non-issue.
-
I'm hesitant to spell out the actual regimen because only your doctor can
evaluate you properly, but it involved Miralax and Colace.
- Lhermitte's Phenomenon
-
This one is apparently uncommon, and though it's somewhat related to the
peripheral neruopathy, it's not the same. For me, it manifests itself as
a curious sensation on the soles of both feet when I nod my head. Really!
-
This phenomenon
is rooted in the spinal cord in your neck, and though my version is really
mild, it can be much more pronounced as it manifests as a shock running down
your spinal cord and down your legs.
-
This was a fun one to figure out: I noticed I had these odd tingles in my feet
but could not figure out what was provoking it, but one evening while watching
TV with my family and my feet propped up on the table, I felt it while I noticed I was nodding my head.
-
Huh?
-
A few intentional nods completely nailed the cause, and it didn't take long before
an internet search showed what it was.
-
My understanding is that it only happens later in the regimen (if at all),
and it's generally benign, but always report it to your doctor if you feel
this head-nodding-provoked sensation. Mine went away shortly after chemo
was done.
-
And to be clear: it was completely painless for me, only interesting,
and absolutely nothing to fear.
- Other side effects
-
There are many other possible side effects, you'll get the whole list
from your doctor and/or nurses, and it's good to keep an eye on this.
-
I am not touching on these other symptoms because they didn't
happen to me, so there's not much I can really offer.
-
But I strongly recommend you make notes of everything you
experience, even if it's not on any list, and report them to
your doctor: your journal will help you get more comprehensive care.
Learning your cycle
Each chemotherapy cycle is two weeks long, with infusion on Day 1,
disconnect on Day 3, and all the rest working your way to the next round.
For me—and everybody is different—the very first days 1 & 2
were no problem at all, and when I saw my oncologist on day 3, I was
thinking: this isn't so bad! For some patients, a mild, low-level
yuck is all they get.
Then the evening of day 3 came and took a nasty turn, and day 4 was
truly miserable. Very unpleasant nausea, overall yuck that lasted all day
spent mostly in bed. I couldn't really sleep, just rested and felt crappy.
The more worrying thing for me: is this just one bad day, or the windup
to a bad week? Thankfully it was the former, with symptoms
winding down on Day 5 (Friday for me), and mostly recovered by the weekend.
The second "off" week was really quite nice, I was pretty much my old
self and was able to participate in a routine life until the next round.
The second round was much like the first in a strictly clinical way,
but because I knew what to expect, that made it much easier. But the
symptoms are cumulative, so round 2 was worse than the first,
and—again—this is where you should be keeping notes for
your doctor.
After one or two rounds, you'll have a sense for what your cycles are
like: How bad are your bad days? When are your bad days? How
is the digestive tract reacting? How are you sleeping?
These are things you get a handle on with experience and with
consultation with your doctors, and with that you'll be able
to plan.
You will definitely find that your whole life revolves
around where you are in your cycle: busy all Day 1, plan for nothing on
Yucky Day 4, and plan on that super fun party on day 12 because you feel
great (or whatever works for you). I have a big red "X" on all Day 4s
in my calendar for the rest of my treatment so I know whether I can
go to that fun party two months from now.
Regarding alcohol; your doctor will probably recommend
avoiding all booze for the first 3-4 days of your cycle: your
body (and liver) are going through a lot, and it's better not
to add more challenges.
My doctor told me I could drink on the "off" week, but I mainly
choose to save that only at the end of that week even though I
feel fine for the rest. I have a weight-loss goal in order to
receive a knee-joint replacement due to arthritis, and the
reduced alcohol has helped.
Nausea and Yuck Control
The doctor will certainly prescribe an anti-nausea medicine,
probably Zofran, but there are others, and if your yuck
produces difficult bowel issues, they'll certainly help on
that front too.
Zofran pills are available in multiple dosages
(4mg and 8mg, at least), plus there's a version
that you can dissolve under your tongue if the
nausea is so bad you can't keep your meds down.
I don't care for the dissolve one because it
leaves a lingering taste in my mouth, and I've
never had problem keeping food or meds down.
A number of friends have suggested ginger in various forms:
gum and teas and ale, mainly, and they do help take the edge off the
nausea. And because of the cold sensitivity, taking a hot
ginger-lemon tea is just a pleasant beverage in its own right.
But there is nothing the doctor can give you that will take
away all the yuck, and it's on this topic that your friends
will come out of the woodwork to ask: have you tried cannabis?
I did my first two rounds strictly by the book, and though the
nausea control helped some, the rest of the yuck was just awful.
So with great reluctance I decided to go down the cannabis road,
and I'm very glad I did.
Cannabis is legal in California for both medicinal and
recreational purposes, and both my primary care physician
and oncologist totally approved this: you do what you need
to do on the bad days.
The two main parts of cannabis are THC, which gets you high,
and CBD, which eases nausea and pain. Both work together to
reduce the yuck on the bad days. There are strains and
varieties, but I've not gotten enough experience to know
about them.
My first foray was into edibles, small chocolate squares with 5mg
each of THC and CBD, but I didn't find that it worked well for me.
It takes quite a while to kick in, and I probably just didn't take
enough.
IMPORTANT: You really have to be careful when taking
edibles for the first time, try a small dose and then wait
two hours before trying more. Not kidding.
It's remarkably common for a novice to take something now, take more
after 30 minutes when they don't feel anything, and again after
60 minutes. But at ~90 minutes it all starts kicking in and you
become a local YouTube star dancing on the table in your underwear.
Seriously, first forays into edibles must be done carefully
until you know what you're doing. Ask the dispensary shop for guidance on this.
I hate cigarette smoke, so I tried the vape pens which don't
cause the cough so badly, and this took a while. There's a huge
variety of product in the vape pens, and it was several of them
before I found the right product and how to properly dose myself.
The first time I used a vape pen, I was sucking on it like it was
a really thick milkshake, a large effort that made me think I was
doing it wrong, but it turns out I was doing it waaaaaaaaaaaaay
right, and I got completely blotto within 60 seconds and just
crashed in bed.
It wasn't at all unpleasant, so I see why people do this on purpose,
but it was clear this was way too much for me, and a smaller dose
worked better when the real yuck came around.
Because I didn't know any better, the original plan was not that
far off from just getting completely stoned on the awful Day 4
so I could sleep it off: I hated the idea, but my doctor said this
was fine, and it helped a lot.
Remember: the CBD is for the nausea and the THC high is for the yuck,
and on the bad days you really need them both. Chemo is not just about
nausea.
But as I studied the cannabis market, I kept learning more about it
and trying new products, and I've really dialed it in with a product
that works super well, it doesn't make me cough, and I can actually
work on my Yucky Day 4!
Taking a single hit when I feel the yuck come on is something I
can only barely feel in my head, so it's not like I'm getting high,
but I just feel better. I'll do this several times a day.
The product I like is from a company called "Dosist" (dosist dot com; I won't
link to cannabis sites from my consulting website). They make
a number of blends that mix up the THC, CBD, and sometimes flavors,
but I settled on the "Relief" blend that has a THC:CBD ratio of 2:1.

The vape pen itself has no buttons, you just take a draw like with a cigarrette,
and it delivers a 2.25mg metered dose in about 3 seconds, vibrating slightly
to let you know it's done. There's a kind of vapor expelled, but there is
no "pot" smell left behind for somebody to notice.
It's easy and reliable to use, and this blend has been perfect for me,
and I am encouraged that it will make my remaining rounds easier.
I've also started with the Dosist "Sleep" blend, which is mostly THC,
and it does a great job of putting me out at night so I get a good night's sleep.
The added THC makes me cough more than the "Relief" blend, but this stuff
has just been easy and reliable.
As with the edibles, I also think it's a good idea to practice this the first time
when you feel good: you need to know how your body reacts to
this new medicine, what dose to take, and how it makes you feel.
Doing this for the first time while in mid-yuck means it's harder
to get that know what caused what.
But unlike edibles, the vape takes effect right away, within a couple
of minutes: you don't need to wait two hours to take a second hit if
the first one didn't do anything. It's best to ask your "budtender"
(the person behind the counter at the dispensary) for advice as a
newbie
Having a trusted friend at hand is a good idea too, just to keep
an eye on you (perhaps with camera at the ready!).
Update for Round 12: the peripheral neuropathy has gotten really
uncomfortable, and I tried rubbing in a CBD-based balm, but
it made no difference after repeated attempts. I don't know if
a THC-based balm would make any difference but ought to try it.
Online research suggests that smoking/vaping of various kinds of
cannabis might help, but it's not bad enough for me to go there; I've
not vaped since day 5 of my 12th round.
"The Stigma"
Side note: I've never done recreational drugs in my life, and
the casual tone above - taking a hit, getting stoned - did not
come easily to me. I was very uncomfortable with the whole
concept, the stigma was strong with me, but I really just got over
it.
It helps me, it's medicine that my doctors approve of, and that's all what I care about.
When I'm on the Bad Day and a hit makes me feel better, it does not cross my mind
that I'm doing something wrong. Holy crap no.
I got comfortable enough to post this on Facebook, which was
a fun conversation to have with my friends; I got 100% support from everybody.
Perhaps you're in a position where you can't be seen
going down this road; I hope you find a way to do it
privately.
As of Oct 2018, I haven't used cannabis since day 4 or 5 of my final
round, and don't expect to again: I was thankful it was available to me,
but it's not something I care to use again.
Random tidbits
Not everything exactly fits in a category, so these are just some notes
in no particular order; I wish I'd known a bunch of these things.
- Insure you have nausea meds before your first infusion.
- Virtually all chemotherapy patients need antinausea
medicine on hand at home—Zofran is very popular—but it
requires a prescription.
-
This is an automatic part of the new-patient intake system for
just about every oncologist, but balls do get dropped,
possibly putting you in an unhappy place if the IV Zofran wears
off on Day 2 and that's your bad day.
-
If you don't have an anti-nausea prescription by the time you're
making your first infusion appointment, ask the nurse and
follow up until you get the Rx. Be persistent about this until you
either have an Rx in hand, or receive a satisfatory explanation of
your alternatives (aka: until you're sure they haven't just dropped the ball).
- Protecting your port in the shower
- The requirement to protect your port from water makes
showering more of a hassle, and unless you can go 3 days
without a shower, you're going to have to find a way to
do it.
- There are many ways to protect your port, but I have found
what works well for me: large clear-plastic water barriers,
and they're easy to order from Amazon.com:
-
-
I put the 7" square right over the port, then put the 9" one fully covering that, then
push all around to make sure it all sticks. You do have to stretch around to make sure
that (say) reaching up to wash your hair won't tear stuff loose, but you'll get used
to this over time.
-
These particular Shower Shields work well.
- Shower just before you head to infusion
- This is all highly subject to your own personal
practices, but I'm a shower-before-bed kind of guy.
-
The requirement to protect your port makes that more difficult,
so I always shower just before I leave for infusion at
7AM. This will last me through the day and night, so I'll go
the hassle of a shower on Day 2.
-
Then, after disconnection on Day 3, I come home and enjoy
a nice hot shower. You don't have to protect your port after
disconnection.
-
As I get better with the hassle, I do sometimes take a shower
every day, but it's nice to not have to.
- Know your 46 hours
-
 That's the infusion time on the take-home pump,
so it means that once your pump is connected, you'll
show up 2 hours earlier, but 2 days later.
That's the infusion time on the take-home pump,
so it means that once your pump is connected, you'll
show up 2 hours earlier, but 2 days later.
-
Example: pump hooked up at 12:30PM Monday, disconnect 10:30AM Wednesday.
-
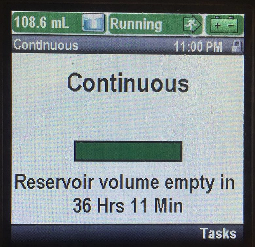
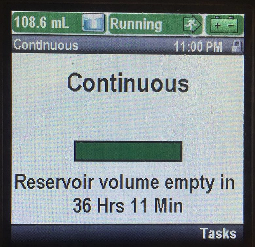
Some pumps show the time remaining (see image to the right), but my first pump did not,
and the Day 1 nurse didn't tell me about this or do the math. So I
showed up for my disconnect appointment with an hour remaining,
making me cool my heels until it expired.
-
It wasn't a huge deal to waste an hour, but it was completely avoidable.
That never happened to me again.
- Get dental work done before chemo
-
Your doctor will probably tell you to avoid non-emergency dental
work, including routine cleanings, while you're undergoing chemo.
Dental work causes systemic infections surprisingly often, I suspect
because poking around in gum sockets where there's bacteria festering
is likely to make its way to the bloodstream.
- Because your immune system is compromised during chemo due to
the reduced white blood cell count, it's wise to move up your
routine cleaning before you start chemo.
Post Chemo
I'm writing this in October 2018, roughly 3 months after my last round - I feel great!
One of the first things I noticed was how great it is to regain control of my own schedule.
During chemo, everything revolves around your two-week infusion cycle, so it's hard
to plan events: will my friend's birthday party six weeks from now be during the "off" week?
Will I get deferred a week for whatever reason, throwing the rest of the schedule off?
I still have medical appointments now and then: I expect blood tests every three months,
plus a CAT scan every year to make sure stuff hasn't come back, but it's much, much
more of an ordinary life now. You just can't imagine how great it is to regain control
over this part of my life.
Around five weeks after my last round, a final blood test confirmed that I was in good shape—including a
nice low CEA value—my doctor ordered removal of my port. They don't do this if there's some chance
I'll need another course of chemo (which sadly does happen for some folks).
Surgery was quick and relatively painless, and I got to take the port home (where I thoroughly cleaned it!).
The port itself is just a hair under 0.5" deep, and the removal scar was tender for a while.
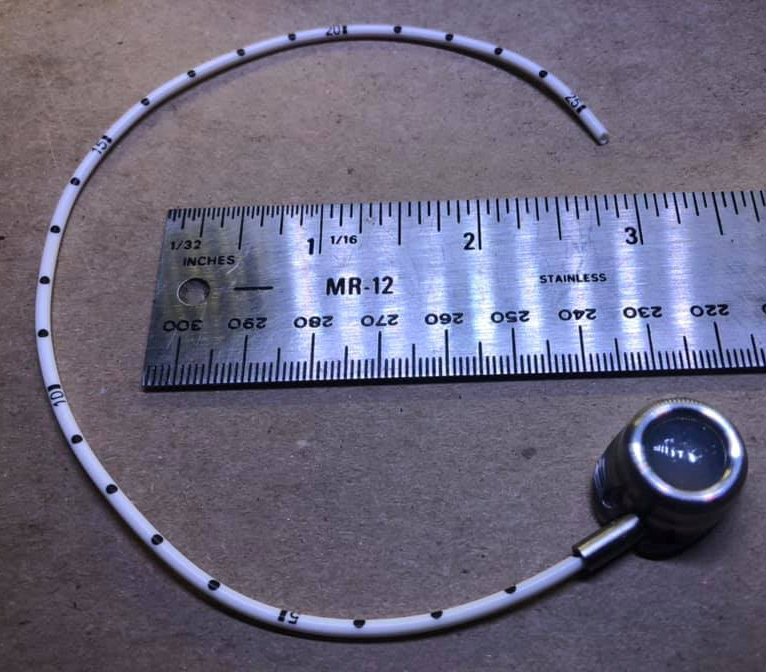
As I had been calling it my "USB Port" the whole time, including on the day of implant, I
followed through by getting a tattoo to "label" the port just above the removal scar:
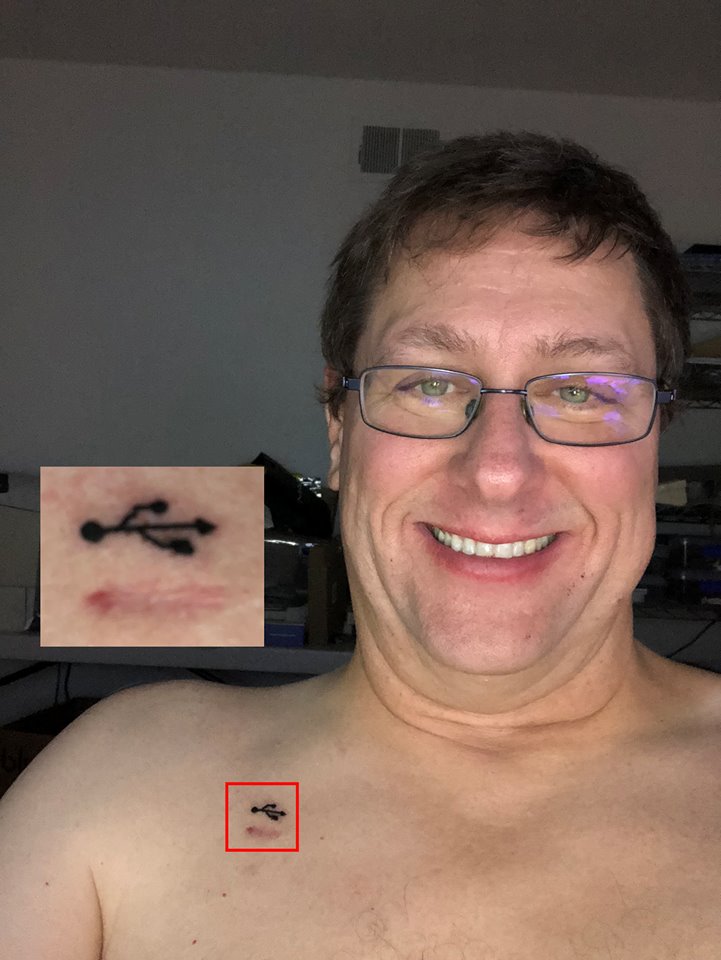
I've never been the tattoo type, but this just felt right. I've gotten no pushback, and I
enjoy rocking out my geek nature.
That aside, the only real lingering effects are the peripheral neuropathy, the tingling and/or deadness
in my fingers and toes. It's unpleasant but mostly doesn't impact my day-to-day life. My physician
has had me try gabapentin, and then the crazy-expensive pregabalin (Lyrica), which so far aren't making
any difference. This may be one of those things I have to live with until it fades away.
Stay Positive
You'll hear this from everybody, but it's true: a positive attitude
makes a big difference, and it can literally save your life.
I'm fortunate that I'm naturally optimistic, I say the glass is
two-thirds full, so it came easy to me to be upbeat during this
whole process, especially since this is only "insurance" chemo
because they don't think I actually have cancer.
Those with more difficult diagnoses, especially Stage 4, may
well not have the same underlying glowing future, and even
the most optimistic person will find it hard to be chipper
on the bad days.
The best way I found to stay positive is to regain as much control
of the process as I could, mostly revolving around understanding
everything. Knowledge is power (and empowering), and I'm fortunate
that I have a high capacity to absorb it.
Also, mysteries are scary, so if you find yourself
worrying about something you don't understand, ask!
Almost all oncology centers can refer you to a support group; I
didn't feel like I needed one, but others I know have found them very helpful
because you're not so alone when you're not the only one. And getting
practical tips for daily living, especially for the more advanced
cancers, will improve your quality of life. Plus, you get a chance
to help others.
Remember: if you bail on chemotherapy before your prescribed
rounds are over (normally FOLFOX is 12), you've reduced your
prognosis. Do what you can to find a way to stick with the
program.
Update: mid-January 2020
Previously I updated things in line, but will start doing it down here so it's easy to find the changes
(no fun to have to scan pages looking for something new).
First: I'm doing great. All post-chemo scans and blood tests have come back negative, and it's been clear that
other than routine monitoring for a while, this cancer is behind me. I'm very grateful for this.
I've also been grateful for the many notes I've gotten from fellow warriors as they share their own experiences.
It's odd the things that bring people together, right?
Some notes and tidbits:
- My Port
- Though my experience with the port was really good, not everybody's is. One of my pen pals, T., had
so much pain from the port that infusion was put off until it could be removed and reimplanted on the other
side, where it was much better. The doctors never figured out what caused this, but it's the first I'd heard
of it. I'm sorry she had to go through this.
- CEA Blood Tests
- I've been asked about my CEA numbers, and they've been great.
-
The CEA blood test look for a tumor marker for
colon cancer, and I have this test done around every four months (along with an annual CAT scan w/ contrast). Anything
below around 4 µg/L is considered normal, and mine have consistently been in the 1.1 range, which says "no cancer".
-
What it's mainly looking for, I understand, is whether any of cancer cells that should have been fully
removed by surgery (or quashed by chemo) might have wandered about and taken root somewhere else, and a rising
number suggests that.
-
One friend, E., has had her CEA in the range 6-12, and it's had the doctors concerned, but they can't find
where it's coming from and it's completely asymptomatic, so apparently they're in wait-and-see mode.
-
But another dear friend S. in stage 4 had her number in the hundreds, and her story ended very sadly.
- NOTE: CEA is not used as a screening or detection test for colon cancer; it's not reliable enough
(some colon cancers do not throw off this marker), so you can't replace a colonoscopy with a blood test. Dang!
-
Still, with all these caveats, it's the first number I look at in my blood work, but I always review all
my test results with my doctor. So should you.
-
- Peripheral Neuropathy
-
The tingling in my hands is essentially all gone, I have to think really hard to detect it, and even then it's nothing.
-
My feet are a little worse, and this only manifests itself at night with the bedsheets on my feet. It's so minor that
I mostly don't think about it, and as far as I'm concerned, this is a non-issue in my life. This tells me that my
doctor threaded the needle properly on the Oxaliplatin dosing.
-
I have no cold sensitivity of any kind.
- Donuts!
-
I really feel like I have to re-emphasize the benefits of bringing donuts to your oncology center
to share with the staff (mainly nursing staff).
- The first time, of course, you need to pay attention to how the process works and to get
the lay of the land: you'll be there for a few hours and will get a sense for who's who and
how the place works.
-
But on your second visit, consider stopping into a local donut shop and picking up a dozen
that you present to the staff. I always got a box with ½ regular donuts, and ½ premium, and
it's hard to overemphasize how much they appreciate this.
-
Always take care of people who take care of you.
-
Nurses will take care of you whether you're nice to them or not, but it makes the world a better place
when you're nice to nurses (my sister is a nurse).
-
Really: this is a big deal, and the Universe will thank you.
Update: Jan 2022
It's been a long time since my last update, but I'm doing great. CEA test this month showed 0.6 ng/mL,
which is down in the basement, I get another CAT scan in March, and once COVID calms down I'll be
getting a followup colonoscopy.
And the end of this year will mark 5 years with no evidence of disease, which is the usual
point where the onco docs say I'm done. Really glad to be here.
- Pandemic impacts
- It's clear that the coronavirus has changed everything, including protocols for chemo patients.
I understand that most places don't allow visitors during infusion, and though it wouldn't have made
any difference to me, this is a big deal for many who need more support.
- In addition, those undergoing chemo have reduced immune function, so all the responsible things
(masks, social distancing, staying at home) are doubly important. Some patients might choose to
completely self-isolate, which may include those in the same household.
-
It's a scary time; please get vaccinated if you can.
- FOLFOX for bile-duct cancer
-
I had a pen pal note that his father in law with bile-duct cancer was just switched to
FOLFOX, something I'd not heard of before. D: I have him in my thoughts.
- Peripheral neuropathy update
-
The tingling in my fingers and toes had continued to decline steadily since I was done
with chemo—side effect of the oxaliplatin—and though in my hands it's
essentially gone, for unknown reasons my big toes have become noticeably more sensitive
-
This is just in the last few days, and though it's not impacting my life, I can tell
something is going on; I'll be letting my physician know about this on Monday.
-
Note that this is almost certainly not gout,
which mainly impacts the joints: this is not that.
-
This might just be normal variation in ongoing symptoms, but with an extra sensitivity
to any symptoms during a time of pandemic.
-
Nothing about this concerns me.
- Soreness after port installation
- Expect your port to be red and sort after implantation surgery: it probably won't hurt immediately after
due to the local anesthetic, but this is still surgery and anesthetic wears off and it's going to be sore and maybe
even red and angry.
-
This is normal, though complications do happen and you should keep your eyes out for it getting worse,
or if it appears to be getting infected. When in doubt, contact your doctor (helpful reader M. suggests
texting a picture).
- "First Bite Syndrome"
-
I updated the side-effects section to include new-to-me First Bite Syndrome, which is pain in
the jaw while taking the first bite of food. I heard about this from helpful reader H., and
later reported to me the same day by reader M.
-
See above for more info, but this is probably in the same category as cold sensitivity:
unpleasant feelings at the start of each cycle that go away later in that cycle.
- Vitamins and supplements
-
It's important to tell your doctor (or onco nurses) about all the meds you're taking,
including over-the-counter supplements. Most will be fine, but you'd hate to find out
that some seemingly-innocent supplement was interfering with your particular regimen. Surprises
are not uncommon.
- "Butt Paste"
-
As noted above, there's almost no way to go through this without the digestive system
ending up in an uproar; for some (like me) it slows things down but for others it
speeds things up and they spend a lot of time in the bathroom. Neither one is fun.
-
Helpful reader M. has noted that Boudreaux's
"Butt Paste"—a great product name if I ever heard one!—has been a lifesafer. Nominally meant for
diaper rash, it's soothing and does the things you would expect in circumstances like this.
-
I haven't used it myself but have some on order for my next colonoscopy prep.
- Cost of Neulasta - it's crazy expensive
-
Fellow patient M. asked me what the heck this crazy line item was: "Injection Pegfilgrastim 6mg" for about $15,000 (!).
This is Neulasta, it's crazy expensive, but that's just the retail price: her carrier paid less than $4k for it
due to negotiated rates. Still very expensive, of course, but it's an amazing molecule and will get you
which is still very expensive. But it's an amazing molecule that does a really good job at keeping your
white cells up.
-
Low white counts make you more susceptible to infection, and if you go into an infusion
cycle with low counts, you'll be deferred. Nobody wants this process to drag out any longer
than necessary.
- Support Groups
- I noted in the main part of this paper that I didn't really see the need for a
support group for myself, and I'm going to amend that somewhat.
-
As far as emotional support, I always felt completely comfortable with my circumstances,
was never concerned about my outcome, and had a very large circle of family and friends to help
me through. I don't remember ever feeling alone or worried - I'm just a really positive guy.
-
On the other hand, process support can be useful: the mechanims of chemo, navigating insurance,
managing symptoms, I could have benefitted from being in a community with others who had
been there already.
-
Actual medical advice should be sought from medical professionals, but having a place to ask
"Is this normal?" during a chemo round might have been helpful (in fact, this is one of the reasons
I wrote this paper in the first place).
-
So: finding a support group—even an online one—would serve both of these purposes
well, and I'm going to encourage everybody to find one.
-
This is especially the case for a private support group, where you'd be able to speak
freely about your journey that you would not do in public. This includes being able to have
indelicate discussions about the effects of traumatic surgery on your digestive tract.
-
Those going through FOLFOX (or spouses) are welcome to contact me; I might be able to
help you find a resource.
Update: Jul 2023
I'm behind on this update, but all is well.
Since my adventure, all scans - both CAT and bloodwork - have shown no evidence of disease, so
in Dec 2022 my oncologist discharged me from his care: I was no longer a cancer patient.
And after a colonoscopy in March 2023 that included the removal of two unconcerning polpys,
I'm now fully 5 years clean post diagnosis.
I expect to still have CEA blood tests once a year or so, plus colonoscopies at whatever interval
my doctors tell me, but at this point I'm now a civilian again :-)
I'm grateful for the support I've received from my family and friends, but I have to
say that being able to help others via this Tech Tip, plus the many emails I get, have
been good for me also.
Unless something big changes, I'm unlikely to post many updates going forward.
Thanks for following.
If you or a loved one is on this same journey, I welcome your emails
with questions or comments.
Grammar note: My use of singular they
throughout as a gender-neutral singular pronoun is intentional.
First published: 2018/04/18 (my Round 8 Day 2)
Updated: 2023/07/29
![[Steve Friedl Logo]](/images/unixwiz-logo-140x80.gif)
 In November 2017, a routine screening colonoscopy revealed
colon cancer—an unhappy surprise in anybody's book—and
I had my sigmoid colon removed in December of the same year
by a very talented colorectal surgeon. Thanks, Dr. Rad!
In November 2017, a routine screening colonoscopy revealed
colon cancer—an unhappy surprise in anybody's book—and
I had my sigmoid colon removed in December of the same year
by a very talented colorectal surgeon. Thanks, Dr. Rad!
 You should of course consider all legitimate treatment
courses, but I'm firmly in the camp of science and modern
medicine, so I thank the giver of this advice for caring about
me so much, and letting them know that I am very comfortable
with my decision given that I really do understand this stuff.
You should of course consider all legitimate treatment
courses, but I'm firmly in the camp of science and modern
medicine, so I thank the giver of this advice for caring about
me so much, and letting them know that I am very comfortable
with my decision given that I really do understand this stuff.
 That's the infusion time on the take-home pump,
so it means that once your pump is connected, you'll
show up 2 hours earlier, but 2 days later.
That's the infusion time on the take-home pump,
so it means that once your pump is connected, you'll
show up 2 hours earlier, but 2 days later.